Disease Screening
Some organizations also recommend HPV screening in certain populations during the Pap smear. Fecal occult blood is detected by microscopic analysis or by chemical tests for hemoglobin in the stool. People with blood in their stool may have a cancerous growth indicative of colorectal cancer. The test requires collection of 3 stool samples that are examined under the microscope for blood.
An Introduction To Painless Products Of Healthcare
The needle that goes into your vein is attached to a small test tube. The person who draws your blood removes the tube when it’s full, and the tube seals on its own. If you’re getting a few blood tests, more than one test tube may be attached to the needle before it’s withdrawn. A blood product called CK-MB is released when the heart muscle is damaged. High levels of CK-MB in the blood can mean that you’ve had a heart attack.
Uncomplicated Healthcare Secrets – What’s Required
For some blood glucose tests, you have to fast before your blood is drawn. Other blood glucose tests are done after a meal or at any time with no preparation. The basic metabolic panel is a group of tests that measures different chemicals in the blood. These tests usually are done on the fluid part of blood.
Prostate cancer, for example, is a very slow growing tumor in many men, but very rapidly progressing and lethal in others. These differences in DPCP exaggerate the apparent benefit of screening, because there is a greater chance that screening will detect subjects with long DPCPs, and therefore, more benign disease.
- If your pituitary gland is not working properly, it may not send out normal TSH amounts—and if this is the case—the thyroid may be healthy.
- What’s considered low or high for you may be normal for someone else.
- The medicine recommended for you will depend on things like how high your blood pressure is, your age and your ethnicity.
- However, if the amount of TSH is off, the thyroid won’t make the right amount of T4.
- The only way of knowing whether you have high blood pressure is to have a blood pressure test.
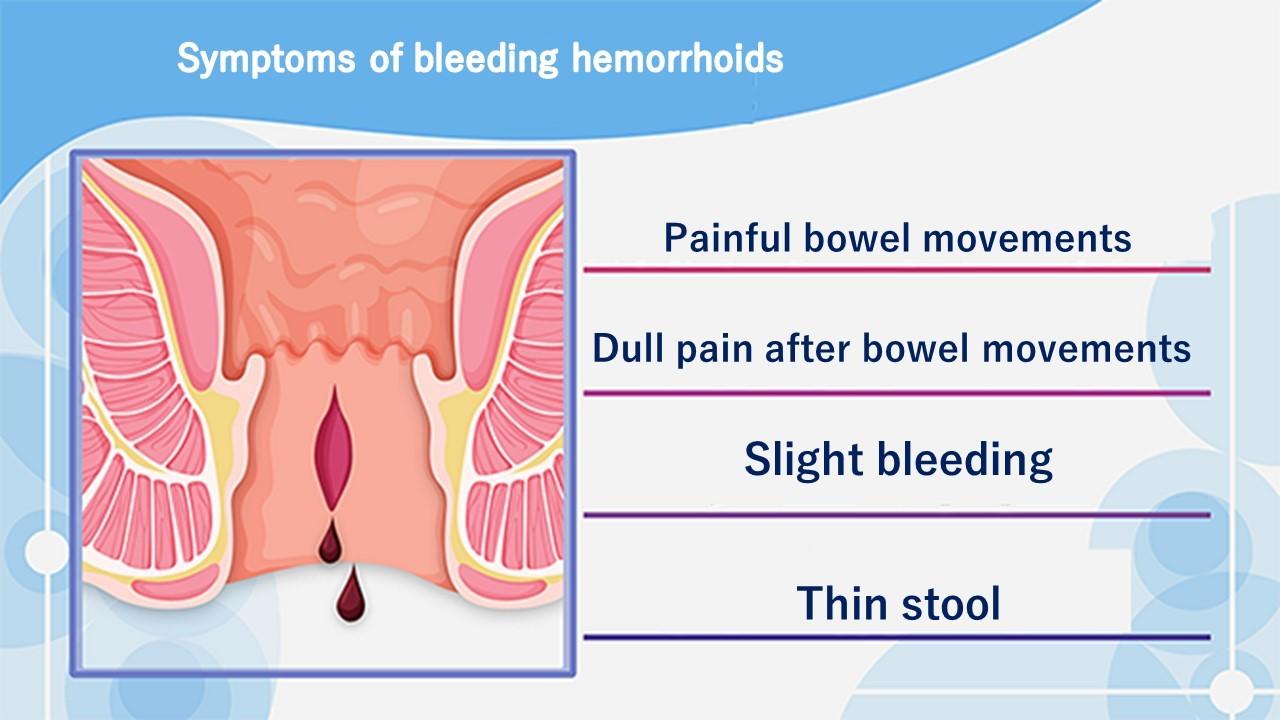
It is important to understand that when blood is present in a stool sample, it can be due to other noncancerous factors, such as certain medications or foods, gastrointestinal bleeding, or hemorrhoids. Testing is recommended starting at age 50 by many organizations including the American Cancer Society. This section presents the result ranges for some of the most common blood tests. Your doctor should discuss any unusual or abnormal blood test results with you. Blood tests show whether the levels of different substances in your blood fall within a normal range.
For an interesting perspective, see the following essay, Link to “What’s Making Us Sick Is an Epidemic of Diagnoses,” in the New York Times by Gilbert Welch, Lisa Schwartz, and Steven Woloshin. illustrates the yield if the screening program were conducted in users of intravenous drugs, in whom the prevalence of disease is 20%. With the same sensitivity and cbd oil specificity, the positive predictive value is 98%. illustrates the yield if the screening program were conducted in males in a clinic for sexually transmitted infections, in whom the prevalence of disease is 4%.
The tests can give doctors information about your muscles , bones, and organs, such as the kidneys and liver. The fluid is used to measure different substances in the blood. The results can help detect health problems in early stages, when treatments or lifestyle changes may work best. Compute the sensitivity, specificity, and positive predictive value of each screening test and comment on the utility of the newer DNA test compared to the previous standard testing. The length of the DPCP can vary substantially from person to person.
With the same sensitivity and specificity, the positive predictive value is 89%. To illustrate the effect of prevalence on positive predictive value, consider the yield that would be obtained for HIV testing in three different settings. The examples below show how drastically the predicative value varies among three groups of test subjects. Positive predictive value focuses on subjects with a positive screening test in order to ask the probability of disease for those subjects. Positive predictive value is the probability that subjects with a positive screening test truly have the disease.
The premise of screening is that it allows you to identify disease earlier, so you can initiate treatment at an early stage in order to effect cure or at least longer survival. Screening can give you a jump on the disease; this “lead-time” is a good thing, but it can bias the efficacy of screening. The two subjects to the right have the same age, same time of disease onset, the same DPCP, and the same time of death. However, if we compare survival time from the point of diagnosis, the subject whose disease was identified through screening appears to survive longer, but only because their disease was identified earlier. These include correlational studies that examine trends in disease-specific mortality over time, correlating them with the frequency of screening in a population.





